At-A-Glance
- Chronic cough (lasting more than 4 weeks) is an extremely common problem, and there are millions of Americans who go from specialist to specialist to specialist without getting any relief (the chronic cough enigma).
- The single most common cause of chronic cough is reflux. More specifically, LPR, also known as respiratory reflux AND notably, LPR is the cause of many other respiratory diseases, as well. Chronic coughers usually have silent reflux, which means they do not have heartburn or indigestion.
- Neurogenic cough is the 2nd most common type of chronic cough. The word “neurogenic” means “nerve-caused.” The term “sick nerve syndrome” is also used because inflammation or injury of the 10th cranial nerve, the vagus nerve, is a common cause of neurogenic cough.
- Notably, more than half of people with chronic cough have both reflux-related and neurogenic cough and BTW, reflux makes neurogenic cough much worse.
- Reflux-related and neurogenic cough are both treatable and both can be cured. However, it usually takes months or years to completely eradicate both. But it’s important to do that work, especially if it’s reflux-related.
The story of chronic cough in this cartoon may look familiar to a lot of you. It’s by Liza Donnelly, a cartoonist for The New Yorker, commissioned by me.

Are you a part of the chronic cough enigma? If you ask your doctors about your chronic cough and they consider it a mystery, you might be.
Or do they assuredly tell you it’s asthma, allergies, reactive airway disorder, prescribe you medications that do nothing, then suggest more / different meds?
I’ve treated thousands of patients with chronic cough, many times ending (or dramatically reducing) decades of incessant coughing after a single week. Read on to understand how.
“Non-Pulmonary” vs. “Pulmonary” Chronic Cough
Right up front, it is worth making the distinction between non-pulmonary and pulmonary cough.
If you are a long-time smoker with a cough, that’s a pulmonary cough because the inflammation and infection in the lungs is real. Other lung diseases (e.g. asthma, bronchitis, emphysema, idiopathic pulmonary fibrosis) are pulmonary. If you have a cough while you have bronchitis, that’s pulmonary. If you have a cough two months after finishing treatment for bronchitis, that’s not. (PS – I believe millions of Americans are over-diagnosed with asthma.)
Nevertheless, I cannot help but point out that all of these pulmonary diseases can be caused by, accelerated by, worsened by respiratory reflux. That discussion is beyond the scope of this post – see the blog on COPD, for example.
There are various causes of non-pulmonary cough. Issues with your stomach (like acid reflux, which is discussed in this blog), certain blood pressure medicines (ACE inhibitors), aspiration due to a too-open larynx (e.g. vocal cord paralysis), and a host of other anatomical and congenital conditions.
Reflux-related and neurogenic cough are the subject of this post, and both are considered non-pulmonary.

The above framed needlework was a gift from a patient, and it hung for all to see near the front door of my office.
Here’s the story: An 80-year-old woman came to see me with a 60-year history of chronic cough. She coughed all day, every day. She had never been to a theater or restaurant. Thankfully, she was married and had friends with whom she played bridge. She went to the grocery store, for example, and did go to the grocery store and did get out of the house at least once a day.
I examined her and she had partially paralyzed vocal cords (vocal fold paresis) but no findings of reflux. I asked her if she’d ever heard the words “neurogenic cough.” She had not. I placed her on a small dose of amitriptyline to take before bed. When I called her the next day, I asked her how she was doing, and her cough was gone, vanished… a correct diagnosis and one pill.
She had her life back and was out enjoying the world. At a follow-up visit six months later, she still had no cough.
Diagnosis of Reflux-Related and/or Neurogenic Cough
Before going into details, let me offer a disclaimer that the quizzes below are generally correct. That is, these quizzes in and of themselves cannot make a positive diagnosis. They can, however, suggest the correct diagnosis. Each of the quizzes has a different purpose and looks at a particular aspect of your symptoms to try to make a diagnosis. These quizzes are validated, peer-reviewed, diagnostic instruments.
The Koufman Chronic Cough Index (KCCI)
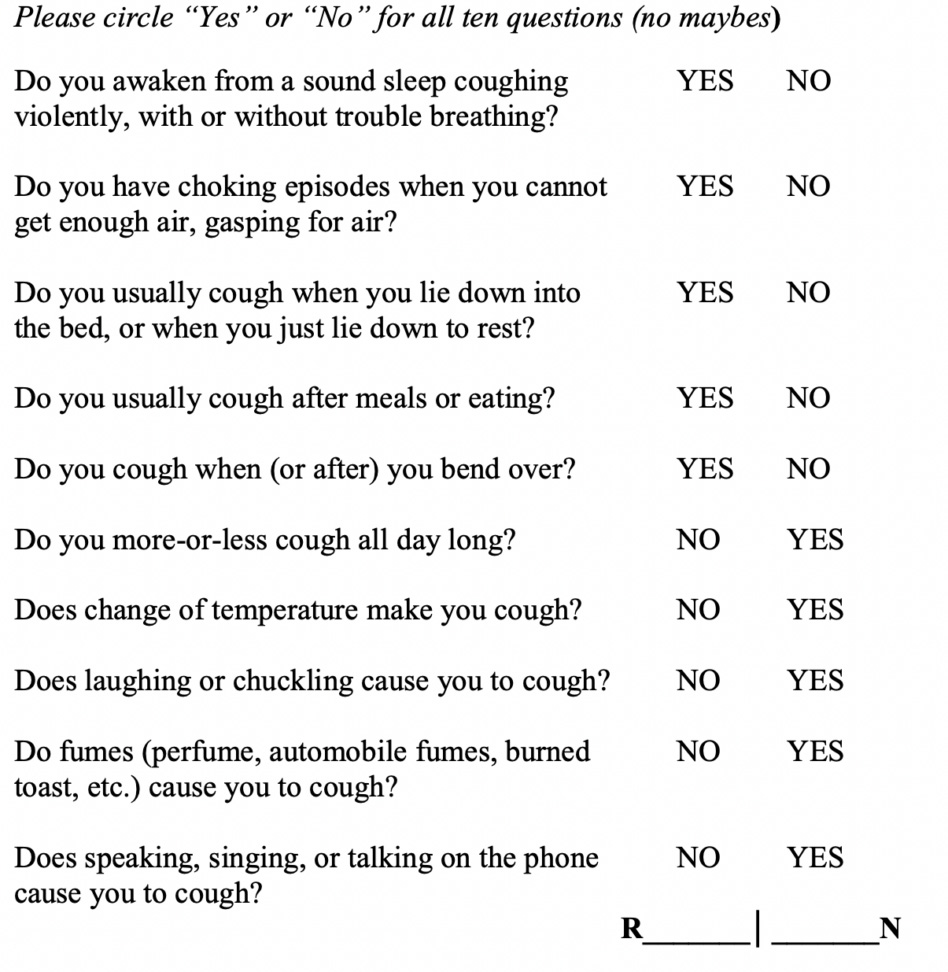
Now, add the two columns to derive the Reflux-to-Neurogenic ratio (the two will always add up to 10.)
If your R:N ratio is 10:0 (or even 9:1 or 8:2), you most certainly have reflux as the primary cause of your cough. Conversely, if your R:N ratio is 0:10 (or even 1:9 or 2:8), you most certainly have a neurogenic cough. All other scores imply that you probably have both reflux-related and neurogenic cough. Remember, neurogenic means “relating to a nerve, the vagus nerve, in this case.
The Glottal Closure Index (GCI)
Certain voice symptoms suggest a possible diagnosis of partial paralysis of the vocal folds (paresis) or of possible vocal cord pathology, e.g. nodules, polyps. Aspiration due to glottal insufficiency is another common cause of chronic cough, which this quiz helps identify.
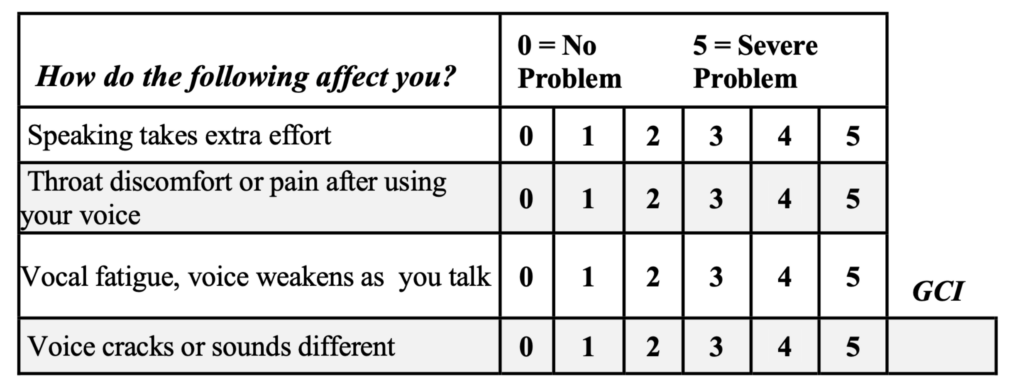
If your GCI is 8 or greater, you are likely to have vocal cords that are not closing properly. This cannot be caused by reflux alone. If you’re a high GCI, it is likely that something has happened to one of both of your vagus nerves, and you should see a laryngologist, that’s a ENT doctor who specializes in laryngeal and voice problems.
Meanwhile, if you do have a high GCI, you may have had a vagal neuropathy, that is, something that resulted in some degree of vagus nerve damage. Just take the quiz and add up the results, and I will try to explain how to reach a diagnosis at the end of this section. Before going on, we should try to figure out whether or not you have reflux.
The Reflux Symptom Index (RSI)
This is another tool to determine if you likely have acid reflux. Note that heartburn and indigestion are just one symptom in the index (which only 20% of refluxers experience).
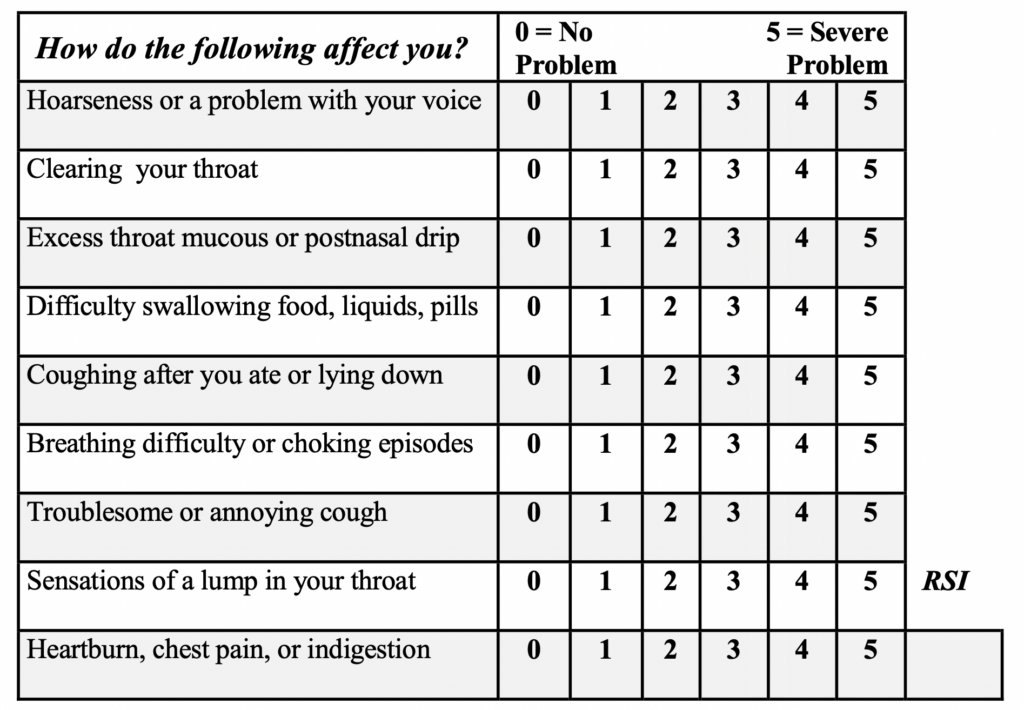
If you have an RSI score of 15 or greater, you have a 90% chance of having reflux, even if you have never had heartburn or indigestion. This is called silent reflux, and it is very common.
Please understand that it’s important to take steps if you have reflux to manage it through lifestyle changes (explained later). If you let reflux run rampant, you’re setting yourself up for sleep apnea, COPD, chronic respiratory conditions, and a far higher risk of esophageal cancer.
Before going further, we have to discuss the vagus nerve and neurogenic cough.
What is The Vagus Nerve and What Does It Do?
Medical students taking anatomy in the first year of medical school spend almost 2 weeks on the cranial nerves. It is likely that the cranial nerves determine who gets an A and who gets a B in the anatomy course. These nerves are special and I need to tell you a little about them, at least, one in particular… the vagus.
There are 12 cranial nerves. Cranial means they come out of the brain and they all have important functions. All of your senses are the result of cranial nerves I thru IX, including the optic nerve, the nerves for smell, taste, hearing, facial movement, etc.
The 10th cranial nerve is called the vagus, with the root word being related to the word vagabond a wanderer. The vagus is longest and most important nerve in the body. Cut both vagus nerves and you are dead.
The vagi control the entire digestive and respiratory systems (except for the diaphragm which has its own nerves). Not only is the vagus a sensory nerve, meaning every symptom you have from these systems comes up the vagus and goes to the brain, but it’s also a motor nerve. It makes everything from taking and swallowing to digesting and bowel function.
Here’s a quiz: Which symptoms are vagal? Nausea, vocal fatigue, sore throat, heartburn, asthma, difficulty swallowing, a sensation of a lump in the throat, cough. The answer is all of them … and more.
If you have the feeling that you have to cough, that’s vagus. When you actually cough, that’s vagus, too.
Post-Viral Vagal Neuropathy (PVVN)
How does the vagus nerve get damaged? They live just under the lining membranes of the nose and throat, so they are susceptible to infection, which can lead to damage that can last far longer than the initial infection.
Common upper respiratory infections caused by viruses can damage nerves in the throat (namely the vagus nerves) that control all respiratory and digestive functions, including speaking, singing, swallowing, reflux, asthma, and cough.
So if you’ve been coughing for months or years, but it started with a cold, the flu, bronchitis or pneumonia, that could very likely be PVVN, and if there’s no reflux, treatment is going to be with amitriptyline and/or gabapentin.
Why Does A Correct Chronic Cough Diagnosis Take So Long?
Part of this issue is due to medical specialization.
The trend towards medical specialization has intensified over the last 50 years… while simultaneously disenfranchising primary care physicians (PCPs). Each specialist – including lung doctors, ENT doctors and GI specialists – just takes care of one part of the body. This has led to specialists who are unable to diagnose / treat reflux-related cough because they don’t understand how the respiratory and digestive tracts are connected. They are directly connected at the upper esophageal valve, which is supposed to protect against reflux in the throat. There is also a direct connection between the throat and the lungs at the level of the vocal cords.
I have taken care of thousands of patients with chronic cough over the course of my career, and almost all have seen multiple specialists including PCPs, allergists, otolaryngologists, pulmonologists, and gastroenterologists.
Without placing blame, the problem is that the go-to specialist for cough should be the pulmonologist, but pulmonologists know nothing about non-pulmonary cough. Without placing blame, the go-to specialist for reflux should be the gastroenterologist, but gastroenterologists know nothing about respiratory reflux can have no test for it. That leaves all of the specialists who deal with the airway without any way to make a diagnosis of reflux related cough.
What to Do About Neurogenic-Related Chronic Cough
Speak to a doctor you feel will be receptive and willing to learn about your issues. Try sharing this blog and/or The Chronic Cough Enigma (I hear about many patients sending that book to doctors, and although that’s certainly not its main intended use, it’s helped many in the past!).
Common treatment options I opted for are amitriptyline in a small dose alone (nightly) and sometimes a small dose of gabapentin (nightly) to start, and attempting to add in more gabapentin to the day, if cough remains. The two medications work together beautifully to normalize the vagus nerve.
If there is neurogenic and reflux-related cough, it’s important to tackle reflux first with a strict 2-week acid reflux detox, then stick with that and move to treating neurogenic.
In my practice, neurogenic cough is usually treated with a combination of amitriptyline (Elavil) in very small doses before bed, as well as with gabapentin (Neurontin), starting in small doses and escalating the dose slowly over weeks or months until the cough is completely eradicated. Unfortunately, there are not many physicians that are skilled in this area, and if you can’t find one, buy a copy of the Chronic Cough Enigma for your PCP and see if he or she will work with you. Failing that, you can have a consultation with me.
What to Do About Reflux-Related Chronic Cough
WARNINGS:
– Don’t take PPIs!
– Understand that acid reflux increases your risk of esophageal cancer, so get screened
Reflux is curable with effort and commitment to change.
I’ve written four books about these topics: Dropping Acid: The Reflux Diet Cookbook & Cure, The Chronic Cough Enigma, Dr. Koufman’s Acid Reflux Diet, and Acid Reflux in Children.
However, here are the most important pieces of advice I can offer:
- No eating or drinking within five hours of going to bed
- Sleep on an incline no less than 45-degrees (gravity helps)
- Eat five small meals
- No fried or high-fat foods
- No alcohol, chocolate or soft drinks (including fruit juice) of any kind
- Take Pepcid 20 mg. before each meal and before bed
- Take a tablespoon of Gaviscon Advance Aniseed after each meal and before bed (not available in stores in the U.S., but available online)
- Drink alkaline water as much as you conveniently can: an alkaline pitcher is convenient (and test it with pH paper or a pH tester to make sure it’s 8.0 or greater)
If you’ve read at least one of my books and you’re following this guidance and you still need help, you can book a consultation with me.