
What is an INLET PATCH and Should I Be Worried About It?
At-A-Glance
- Stomach lining (called gastric mucosa) belongs in the stomach, but some people have ectopic gastric mucosa in the upper esophagus, a so-called Inlet Patch. (Ectopic gastric mucosa means “stomach lining in an abnormal place.”) Inlet patches are found in 2% of people undergoing upper endoscopy (examinations of the throat, esophagus, and stomach).
- Most of the medical world assumes that inlet patches are congenital in origin, however, there is strong evidence that inlet patches are caused by acid reflux, specifically by respiratory (LPR) reflux.
- People with inlet patches are seven times more likely to have (reflux-caused) Barrett’s esophagus (ectopic gastric mucosa in the lower esophagus), and this suggests that the “congenital hypothesis” must be wrong, because an inlet patch is essentially “Barrett’s of the upper esophagus,” caused by reflux.
- In my practice 100% of people with inlet patches have severe respiratory reflux (LPR); and notably, both Barrett’s esophagus and inlet patches are sometimes reversible, that is, they can disappear with prolonged anti-reflux treatment … additional data that refute the “congenital hypothesis.”
- Inlet patches rarely cause symptoms such as globus (as some literature suggests); they usually are asymptomatic, incidental findings. Furthermore, they should not be ablated or surgically removed, again because they go away with tight reflux control.
What Is an Inlet Patch?
You can think of an inlet patch as “Barrett’s of the upper esophagus.” If you have respiratory reflux, and a lot of it, you can develop an inlet patch. This is a small Barrett’s-like area of stomach mucosa just below the esophageal inlet, that is, within the first few centimeters of the top of the esophagus where it connects to the throat, “the inlet.” So what is Barrett’s?
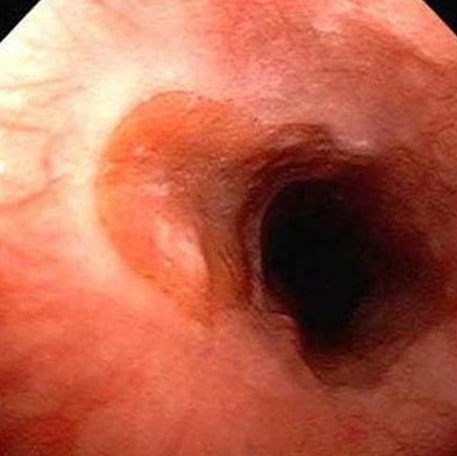
The salmon-colored thumb-print area (left) is an inlet patch. It looks much like Barrett’s esophagus, but the latter is in the lower esophagus, while the former is in the upper esophagus, near its junction with the throat, i.e., the esophageal inlet.
The normal lining of the esophagus is squamous epithelium; however, with excessive and prolonged exposure to acid and pepsin, the esophageal lining can undergo change to columnar epithelium with goblet cells, so-called Barrett’s esophagus, which is stomach lining growing in the esophagus where it shouldn’t ought to be. See my blog about Barrett’s Esophagus.
How Common Are Inlet Patches?
How common are inlet patches? The medical literature generally accepts the 1-2% number; however, inlet patches can easily be overlooked by endoscopists (who mainly wish to view the lower esophagus and stomach).
A group of endoscopist authors looked care fully for inlet patches and found that 14% of their reflux patients had it, and some had multiple inlet patches; in my experience, inlet patches are found in about 10% of my endoscopies.
What Causes Inlet Patches?
Most of the medical literature assumes that inlet patches are congenital, but if that were the case, one would expect to find inlet patches in people without acid reflux … but that is not the case. Indeed, there are data that virtually prove that inlet patches are due to LPR reflux.
First, every patient (100%) in my practice with an inlet patch had/has pH-documented respiratory reflux (LPR). And, I have also seen both Barrett’s esophagus and inlet patches reversed, that is, go away with prolonged, effective anti-reflux treatment. My experience refutes the “congenital theory.”
Second, in a landmark paper, Inlet patch: associations with endoscopic findings, the authors found that patients with inlet patches were seven-times more likely to have Barrett’s esophagus (3.5% versus 0.5%, p = 0.0001). And third, it has been reported that people with inlet patches have worse reflux that other refluxers without inlet patches.
By the way, no one has ever suggested that Barrett’s esophagus is congenital; everyone knows that it is reflux-caused. Indeed, the data show that people with inlet patches and/or Barrett’s esophagus all have severe reflux. Again, I like to think of inlet patches as “Barrett’s esophagus of the upper esophagus.”
Should I Be Worried About My Inlet Patch?
While Barrett’s esophagus is considered a type of esophageal pre-cancer, it rarely degrades to that. There is another step in the pre-cancer progression, dysplasia, which is a kind of disorganization of biopsied cells under the microscope.
In the old days, we told patients with Barrett’s that they had a 1% chance per year of getting cancer, but cancer is actually very uncommon. Having worked with almost 800 Barrett’s patients over four decades, I can report that none (0%) of my patients developed cancer. The reason for this is that reflux causes cancer, not just Barrett’s.
So, if we assume that an inlet patch is essentially “Barrett’s high in the (upper) esophagus,” then what is the cancer risk? A search of the medical literature reveals just a single case of cancer developing in an inlet patch. So for those of you who have Barrett’s high or low, the key is reflux control … all of my work focuses on that; see Silent Reflux and Respiratory Reflux. With a reasonable anti-reflux program in place, don’t worry; be happy; there’s no cancer in your future.
What can be done about your inlet patch? Since the data on inlet patches prove they are caused by LPR reflux, you should try to stop your reflux in its tracks; see Barrett’s and Vegetarian blogs, as well as my books, Dropping Acid and Dr. Koufman’s Acid Reflux Diet.








