At-A-Glance
- The lower esophageal sphincter (LES), the valve between the stomach and the esophagus, normally prevents reflux. But once reflux gets going, the LES can become inflamed, stiff, swollen, and less effective as a barrier. Now you may have GERD, gastroesophageal reflux disease. The more you reflux, the worse the LES functions, and the more you reflux. It’s a vicious cycle and reflux tends to worsen over time. Eventually, esophageal function is compromised, and then the upper esophageal sphincter (UES) fails. Now, you have RR (respiratory reflux) aka LPR (laryngopharyngeal reflux).
- Because Silent Reflux is common (reflux occurring during sleep), you may not have identifiable reflux symptoms. Just the same, your esophagus behaves like the Holland Tunnel with no tolls, not even an E-ZPass; when you lie down — what’s in your stomach — is in your esophagus — is in your throat.
- The degree to which antireflux defenses are compromised will determine what it will take to fix your reflux. I have created four reflux stages: Stage IV: Decompensated, Stage III: Partly-compensated, Stage II: Stable, but vulnerable, and Stage I: Compensated, in remission.
- You, maybe with your doctor’s help, can determine your reflux stage; and not surprisingly, each has different recommendations. Of course, the over-aching goal is recovery, cure of reflux.
Note: Respiratory Reflux (RR) and Laryngopharyngeal Reflux (LPR) are synonyms and the terms can be used interchangeably. But going forward, I prefer the term RR and so should you; it is easier to pronounce, more intuitive, and implies that RR can affect any and all parts of the respiratory system, which it does.
People with acid reflux generally fall into two groups: those with GERD who have esophageal symptoms such as heartburn and indigestion; and those with LPR, who have respiratory symptoms such as laryngitis, sinusitis, shortness of breath, chronic bronchitis, cough, sleep apnea, etc. Why most people have either LPR (75%) or GERD (25%) and not both is unknown; but about 10% of refluxers have both. Notably, most people with the LPR (~80%) have silent reflux, that is, they do not have GERD symptoms; and actually, they may be unaware that they have reflux at all.
People ask me what’s the best treatment for reflux? It depends; the punishment must suit the crime. For both LPR and GERD, reflux has different degrees of severity, but most people seek medical attention when they develop distressing and/or daily symptoms. BTW, ask a gastroenterologist and s/he will tell you that reflux is a chronic disease needing lifelong treatment; but this is not correct; it is fixable.
What Causes Acid Reflux in the First Place?
This is a problematic question because for most refluxers, its etiology and pathophysiology is multifactorial; that means that it is rarely the result of just one cause. Often, people have long-standing, dormant, subclinical silent reflux as a result of dietary and lifestyle indiscretions, and when a precipitating event comes along, the reflux appears to be sudden. This is the last straw principle: when threshold is exceeded, collapse occurs. The “last-straw event” causes decompensation of the reflux-prevention symptom … as evidenced to the sufferer by the sudden emergence of distressing symptoms.
The most common reflux “precipitators” are: (1) viral upper respiratory infection (URI), including a cold, the flu, and Covid; (2) “vacation” or any other episode involving excessive eating and drinking for several days; (3) intermittent or habitual Late Night Eating, snacking, and/or alcohol; (4) a course of antibiotics and/or steroids; (5) ACE-inhibitors (a class of blood pressure medicine); and (6) vagus nerve damage, most commonly Post-Viral Vagal Neuropathy, covered in a Lecture on YouTube … and a topic of a future post, soon.
The single most common precipitants are URIs, big meals late, and too-much alcohol. So the next question is what are the causes of the dormant, not-yet-decompensated state? And the answer is the exact same list as above, plus overeating, obesity, a high-fat diet, and consumption of acidic soft drinks.
The Laws of Decompensation
1st Axiom – Before: The components of a system are in dynamic balance
2nd Axiom – Decompensation is preceded by often ignored and overlooked warning signs
3rd Axiom – The Last straw principle: When threshold is exceeded, collapse occurs
4th Axiom – After: Recovery requires stabilization and repair of all essential elements
Long ago, I wrote Laws of Decompensation to help explain how and why things fall apart; above is a simplified version of the original. (FYI: The definition of “de‧com‧pen‧sa‧tion” noun is the functional deterioration or collapse of a previously working structure or system.) And here’s an interesting thought: while this paradigm neatly apples to acid reflux; it could equally be applied to collapse of a bridge, a business, or even a marriage. Meanwhile, these laws made me think about the stages of reflux and recovery.
The Stages of Reflux and Recovery
Stage IV: Decompensated
Stage III: Partly-compensated
Stage II: Stable, but vulnerable
Stage I: Compensated, in remission
Unfortunately, clinical data cannot always determine the stage of reflux, or even if you have it. When a gastroenterologist does an upper endoscopy; s/he will not know if you have reflux, especially LPR. Indeed, I have previously reported that 88% of people with LPR have normal esophageal examinations. The gastroenterologist can’t help you with LPR, period.
Neither endoscopy or any of the other testing (including reflux testing, impedance) in the GIs bag are reliable diagnostics for you. If you feel that you must see a doctor, an ENT is better choice. Try to find one who is knowledgeable about reflux, and ask before you make the appointment and also ask if s/he does TNE (Transnasal Esophagoscopy).
So, what is the best noninvasive diagnostic test? Ask your primary care physician (PCP) to order a barium-swallow esophagram (BSE) done in the sitting or standing position, as well as lying down. This is a functional examination and can show reflux, upper valve dysfunction (a so-called cricopharyngeal bar), esophageal dysmotility, a hiatal hernia, as well as scar-band rings, some benign and malignant growths, diverticula, and some congenital abnormalities. On BSE, the three of the surest signs of Stage IV decompensation, are free reflux, a cricopharyngeal bar, and poor or disordered esophageal contractions (dysmotility).
In any event, for this post, let’s assume that most of the patients and consults are decompensated refluxers who require medical intervention. But you probably want to know your reflux stage, if it you face any potentially serious consequences, and what to do? Take the RSI (Reflux Symptom Index) Quiz.
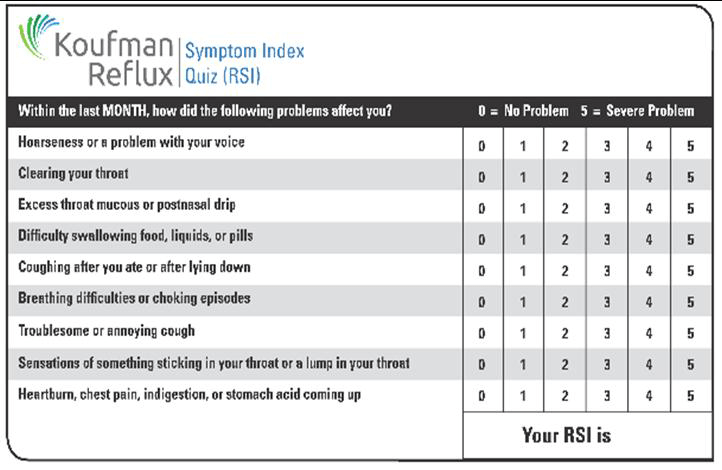
If you have a total RSI of 15 or more (with or without heartburn), you have a 95% chance of having respiratory reflux (LPR). If your score is 25 or more, you are in the championship division! Keep in mind that decompensation is preceded by often ignored and overlooked warning signs and symptoms. In addition to having a high RSI quiz score, check out the red flags.
Red Flags for Respiratory Reflux
Asthma
Airway obstruction
Shortness of breath
Choking episodes
Snoring and sleep apnea
Pneumonia (esp. recurrent)
Chronic bronchitis
Chronic cough
COPD
As far as I am concerned, if you have any of those, you have respiratory reflux until proven otherwise.
Unfortunately, those frightening symptoms are often evaluated by primary care physicians, pulmonologists, and otolaryngologists, all of whom may not think about reflux at all. And if they do, they usually consult a gastroenterologist who knows virtually nothing about respiratory reflux and has no tests for it.
Let me help you; this BLOG has ALL POSTS on the navigation bar. Use it to look for the articles that apply to you; and as a last hope for a cure? I also do Virtual Consultations.
How Does Treatment Vary for Different Stages of Reflux?
The fact that reflux is not a static condition and sufferers differ widely is a problem because of individual variations. People experience different patterns of reflux, with different reflux trigger foods, and different responses to different therapies at different times. If you have read Dropping Acid and/or Dr. Koufman’s Reflux Diet you know that my reflux diet actually has four phases: Detox, Transition, Maintenance, and Longevity. (By the way, I consider that pair of books to be companion books.)
Dropping Acid covers the basics and the science behind a low-acid diet, but it does not cover transition well. Dropping Acid is where it all began, the linkage of three paradigm-shifting words, “Reflux,” “Diet,” and “Cure.” Transition and beyond is better covered in Dr. Koufman’s Reflux Diet, so if you only want to get one book get that one.
Where do you fit, and where do you start? The answer depends upon the stage of your reflux and many variables that are unique to you.
Stage IV (decompensated) People with reflux at this stage need to stop the reflux cold in its tracks for three weeks to three months. This will allow the esophagus and its valves to heal; and yes, that is very much in the range of possibility for you!
Elements of the Reflux Detox Program
Close the kitchen five hours before bed (so that you sleep with an empty, quiet stomach)
Nothing out of a bottle or can except still water; No alcohol … What to Drink?
Low-acid, low-fat diet, e.g., no fried food
Sleep on an incline of 45-degrees (a standard reflux wedge won’t do)
Take Famotidine and Gaviscon Advance Aniseed
Drink alkaline water and use alkaline water spray
Chew gum or suck on a hard candy after meals
All of this detox program is in these blogs: Respiratory Reflux, How to Get Rid of Pepsin, Silent Reflux, Alkaline Water, Gum Chewing, Trigger Foods, Alcohol, and Is It Good to Be Vegetarian?
YOU STAGE IV REFLUX PEEPS … AND THAT’S MOST OF YOU READING THIS … READ ALL THE POSTS
Listen to your body, and when all of your symptoms are under good control, you can move from Stage IV: Detox to Stage III: Transition. Detox must be a minimum of three weeks (to three months); and after detox, it is not all or nothing, that is, after detox, you cannot just go back to things the way they were before … duh!
Stage III patients are just out of the reflux abyss, but still on the edge. You Stage III refluxers are “brittle,” and the word brittle implies that it would not take much for you to fall back into the abyss. So, you must be careful. During the Transition Phase you may start adding back foods, one at a time, and you still must avoid high-risk foods such as chocolate, fatty meats, soft drinks, and alcohol.
Transition extends from the end of the detox period until Stage II. For some people Stage III takes weeks, and for others it can take many months, even a year or so. Part of the Stage III experience is trying to figure out if you actually have specific Trigger Foods.
What do you miss most that you’d like to add back into your diet? Most fruits and vegetables (but no citrus) may be fine to try adding … and some meats, but not too fatty … no cheeseburgers for example. And for sure, not yet alcohol or chocolate. Transition is trial and error, and it can be tricky, so just add one food item at a time. If, for example, you love onions, read the Onion Post. When you no longer have any reflux symptoms, you are in Stage II: Stable, but still vulnerable.
Stage II implies that your symptoms are under control and that you are approaching remission. It also assumes that your trigger foods have been identified and that you avoid them. Obviously if you know that chocolate is a trigger food for you, you need to avoid it (for at least a year). Stage II patients feel confident about their reflux and health; although they still have to plan meals and dine out with thought.
Now, medical treatment may be successfully tapered. Here’s how: decrease one dose of the famotidine each week form 4 to 3 to 2 to 1 to none … discontinue the nighttime doses last. After that, you can taper the Gaviscon Advance. But keep both around to help get you over a bump in the road if you stray from the straight and narrow, e.g., eating too late. If that happens take the meds that evening like before as a preemptive, preventative therapeutic.
Stage I, remission, is the goal … Congrats! This is the stage when people go about their lives without excessive concern for dietary and lifestyle issues. However, this does not imply that relapse isn’t possible. When people are in remission, they still need to pay attention to how they eat, especially when they get out of their regular routine, such as with travel. You have beaten reflux, but that hole in the ground, the reflux abyss, isn’t that far away.
You will need to figure out what works for you, whether you can drink Alcohol, eat dinner later, etc. Every variable in every treatment stage will stay in the back of your mind. And oh yes, going out for pizza and a beer late after the show? That ship sailed … it’s gone.