At-A-Glance
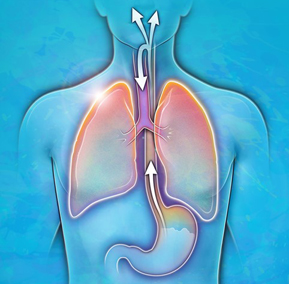
- There are two completely different patterns of acid reflux; one involves esophageal reflux and the other respiratory system reflux. The former is called GERD (gastroesophageal reflux disease); and the latter is called LPR (laryngopharyngeal reflux). (LPR literally means reflux into the voice box and throat.)
- LPR, often “silent” occurring without obvious reflux symptoms like heartburn, is more common than GERD. In fact, there are four people with LPR for every person with GERD. Unfortunately, the “go-to” doctor for acid reflux, the gastroenterologist, has no test or treatments for LPR; they are clueless when it comes to LPR.
- Although there is variation in the reflux training of otolaryngologists, at least ENTs can examine the throat. Silent Nocturnal Respiratory Reflux (aka silent LPR) can affect any part of the respiratory system, and can be easily overlooked. It can, however, be diagnosed by a skilled ENT examiner. Heartburn and indigestion, the symptoms of GERD, are usually diagnosed and managed by primary care physicians or gastroenterologists.
- The differences between the patterns and symptoms of LPR and GERD depend upon differences in diet and lifestyle, especially what you eat and when you eat it. And of course, some people can have both GERD and LPR.
In short, not only are things not what they seem,
they are not even what they are called!
―Francisco de Quevedo
What Are GERD and LPR?
When you think of acid reflux, I’ll bet you imagine a TV ad showing an obese man in a sleeveless shirt, sitting on the sofa watching TV with the obvious remnants of a large Philly-steak sandwich ― and then he leans back, clutches his chest, and moans, right? You think acid reflux is about heartburn and indigestion from eating too-much, too-greasy, too-just-wrong food. That condition, named by gastrointestinal (GI) specialists, is called GERD, gastroesophageal reflux disease.
What if you don’t have heartburn or indigestion, but after a night out drinking, you awake in the morning with “whiskey voice” (gravelly, heavy hoarseness), a ton of throat mucus, sore throat, and a sour taste in your mouth? That’s LPR, laryngopharyngeal reflux. (LPR literally means reflux into the voice box and throat.) I coined the term LPR in 1987, because I felt that we needed a term to differentiate ENT patients with voice, throat, and breathing problems from GI patients with GERD.
There is no way to explain why some people have LPR or GERD other that to examine the reflux risk factors. In general, LPR patients eat and drink too much, too late. And there are some people have both LPR and GERD; I estimate that group to be 15%.
What Is Silent Reflux?
In 1988, Dr. Walter Bo, a colleague and friend came to see me because he was experiencing symptoms including chronic throat-clearing, cough, and hoarseness. After his examination, I told him that he had acid reflux. He laughed and dismissed the idea … because he thought that to have reflux one must have heartburn … and he didn’t have any of that.
He stated categorically that his problem was not reflux. But after I explained that one could have acid reflux without heartburn, Dr. Bo rolled his eyes, thought about it for a minute, and then slowly announced, “I see … I have the silent kind of reflux.” I replied “Yes Walter, that’s it! You have silent reflux.” And thus, the term was born.
So acid reflux all night long (that you just sleep through) while it’s in your throat is silent LPR. And here I would like to introduce a new acronym SNoRR, Silent Nocturnal Respiratory Reflux; and I think that the term is self-explanatory. Today, in the author’s experience, SNoRR is the most common acid reflux pattern today, and it can go on for decades unnoticed; it can even be deadly.
Why SNoRR and not regular GERD or LPR? It depends on what and when a person eats their last meal of the day and whether that dinner is the big refueling (“over-eating”) meal of the day, which it is for most Americans. For example, I recently, I asked a patient what time she ate dinner and she replied 8:00pm; and what time did she go to bed? 10:00pm. Two hours is not enough time for the stomach to empty, and one would expect her to have SNoRR all night, every night, even if she never even once awakened from sleep because of the SNoRR.
To put the names to the faces, and make comments on the patterns, clinical manifestations, and treatments for LPR and GERD; shown below is the nomenclature, the evolution of terms, for acid reflux in use and it the medical literature over the past fifty years.
re·flux n [ L re– back + fluxus flow ] 1: a flowing back 2: a process of refluxing
Common Terms for Reflux
General Terms
Acid reflux
Gastric reflux
Indigestion / Heartburn
Terms for Esophageal Reflux
Gastroesophageal Reflux Disease, GERD
Gastro-Oesophageal Reflux Disease, GORD [U.K.]
Peptic Esophagitis / Esophageal Erosions
Terms for Throat / Airway / Respiratory Reflux
Reflux Laryngitis
“Atypical” Reflux Disease
Extra-Esophageal Reflux Disease
Laryngopharyngeal Reflux, LPR†
Silent Reflux†
Airway Reflux†
Respiratory Reflux, RR†
Silent Nocturnal Respiratory Reflux, SNoRR†
† Terms coined by Dr. Jamie Koufman
Note: GERD and LPR are still the most accepted and commonly used terms in medicine.
Telling LPR from GERD by Symptoms
What are the common symptoms of LPR and GERD? We asked thousands of reflux patients about symptoms, and most had LPR symptoms, not GERD symptoms. And, many people had several symptoms; here are the results of the study:
Post-nasal drip 15%
Chronic throat clearing 14%
Lump-in-the-throat sensation 14%
Hoarseness 12%
Sore throat 1%
Heartburn 10%
Chronic cough 9%
Difficulty swallowing 8%
Choking episodes 7%
Heartburn ranked number six of the nine symptoms. And in another study; we found that LPR patients outnumbered GERD patients four-to-one; 83% never had had heartburn.
Think You Might Have LPR?
Take the reflux quiz below. It is called the Reflux Symptom Index (RSI), and it is a validated research instrument that I developed and reported in 2002.
The Reflux Symptom Index (RSI)
| How do the following affect you? | 0 = No problem 5 = Severe problem | RSI | |||||
| Hoarseness or a problem with your voice | 0 | 1 | 2 | 3 | 4 | 5 | Total |
| Clearing your throat | 0 | 1 | 2 | 3 | 4 | 5 | |
| Excess throat mucous or postnasal drip | 0 | 1 | 2 | 3 | 4 | 5 | |
| Difficulty swallowing food, liquid, pills | 0 | 1 | 2 | 3 | 4 | 5 | |
| Coughing after you ate or lying down | 0 | 1 | 2 | 3 | 4 | 5 | |
| Breathing difficulty or choking episodes | 0 | 1 | 2 | 3 | 4 | 5 | |
| Troublesome or annoying cough | 0 | 1 | 2 | 3 | 4 | 5 | |
| Sensation of a lump in your throat | 0 | 1 | 2 | 3 | 4 | 5 | |
| Heartburn, chest pain, or indigestion | 0 | 1 | 2 | 3 | 4 | 5 | |
If your RSI score is 15 or more, you have a 90% chance of having LPR. And there are other symptoms, not in the RSI that also strongly suggest LPR. These are: (1) “Asthma” that doesn’t respond to asthma medication and during an asthma attach you have more trouble breathing IN rather than OUT; (2) You have a bitter taste in your mouth in the morning; (3) You awake in the middle of the night coughing, often violently and sometimes with choking; and (5) You have loud snoring with or without sleep apnea. (If so, you probably have had SNoRR for years, maybe decades.) See my blog on Snoring and Sleep Apnea and Big Uvula.
Which Doctor Should I See?
Unfortunately, many physicians are still unaware that reflux, especially silent LPR, is the underlying cause of so many respiratory conditions. That said, I recommend that you see an otolaryngologist (ear nose, and throat doctor) if you think you have LPR. Your primary care physician or gastroenterologist is who you should see for symptoms are heartburn and indigestion … but not for LPR. I frequently tell patients that if you have LPR, going to see a gastroenterologist is a waste of time as they have no tests for LPR and they have no idea how to treat it. It’s just not in their curriculum. Likewise the ENT doesn’t have a special test for LPR reflux; today, they make the diagnosis by examination of throat.
Parting Shot: Respiratory Reflux
As terms go, laryngopharyngeal reflux is a mouthful, and it isn’t inclusive enough; LPR literally means reflux into the voice box and throat. But “LPR” reflux can cause problems everywhere in the respiratory tract, including the ears, nose, sinuses, trachea, bronchi, and lungs?
Therefore, I propose that we change the term LPR for the easier-to-pronounce, more intuitive and more accurate term, Respiratory Reflux (RR). For now, I have no problem using LPR and RR as synonyms; although I believe that Respiratory Reflux is a more-inclusive, “pinnacle term” that will replace LPR.
For information about treatment, see my books on Amazon: Dropping Acid: The Reflux Diet Cookbook & Cure and Dr. Koufman’s Acid Reflux Diet. And if you would like to schedule a virtual consultation with me, you can book online.
References
There a numerous references that describe the research that has been done in LPR; if interested see pages 43-49 in my Curriculum vitae.