Can You Cure Sleep Apnea and GERD By Fixing Acid Reflux?
At-A-Glance
- Sleep apnea prevalence has dramatically increased over the past few decades, which parallels the patterns of unhealthy diet and lifestyle choices tied to reflux.
- By controlling and curing acid reflux (LPR & GERD), sleep apnea can be reversed. Details are at the end of this blog.
- I have observed over the past few years that changes in the throat (pharynx), correlated with reflux testing, show that narrowing of the throat with granularity and inflammation is the result of long-standing (perhaps a decade or more) silent nighttime respiratory reflux (also known as LPR).
- These observations, analysis and conclusions have not previously been reported, and for that reason, medical photographs are included in this blog to help physicians make the correct diagnosis and treatment. (If you have sleep apnea, you can share this article with your doctor.)
Curious about how you cure sleep apnea and GERD? For starters, it’s important to understand the connection between the sleep disorder and acid reflux, including silent reflux.
Over the course of my career, I’ve continued to make observations and perform studies that link respiratory reflux to many respiratory diseases, now including sleep apnea.
In my practice, most patients with sleep apnea also had severe acid reflux in their throat, and the correlation appears to be a reliable diagnostic.
It is possible to reverse sleep apnea and GERD with acid reflux treatment, but you need to follow the rules in my bestselling book Dropping Acid strictly enough to consistently prevent silent nighttime respiratory reflux.
How Acid Reflux (GERD) and Sleep Apnea Are Connected (Technical Section)
A 38-year-old came to see me with complaints of excess mucus, chronic throat clearing, and a sensation of a lump in the throat. On examination, he had findings of long-standing silent nighttime reflux. In particular, the caliber of the barrel of his throat was narrow and the lining membranes were thick and inflamed (see below).
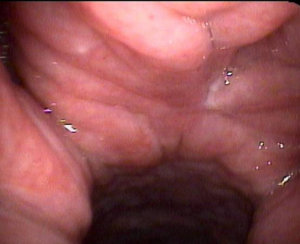
While I do not usually put medical photographs on my blog, in this case, two pictures are worth a thousand words. On the left is a normal throat looking from the top down (from the back of the nose all the way down to the vocal cords). This is normal!
This examination and photographs like this are taken by ear, nose, and throat physicians using an ultra-thin tube with a lighting fiber and camera on the end. It then is placed through the nose without pain. Your family physician or others do not usually perform this specific examination. It is an ENT exam. (I took the above photos.)
The photograph on the right is taken from the same spot high in the nose and looking down the patient’s throat. The findings are severe granularity, inflammation and narrowing from the back of the nose all away down to the voice box.
I asked the patient if he has sleep apnea and he confessed that he did. I also asked if he snored loudly, and he told me his wife made him sleep in another room.
I want to show you why this patient (and maybe you) snore, but before I show you those photos, let me talk about the palate and uvula.

The uvula is the little thing hanging down from the front of the palate seen here in its normal configuration and size. This is a view from the front. A normal small uvula is not seen with the examination that I use with my little examination tube that I place through the nose (these photos are seen from this angle, from the back).
Here are two examples of patients with silent nighttime reflux and large uvulas. The one on the right is gargantuan and resting on the epiglottis, which is part of the larynx. These people snore. (The photograph on the right is actually taken from the patient described above.)
For years, ENT surgeons have been removing parts of the palate and uvula as a surgical treatment for snoring. This is called an UPPP. While this procedure can stop snoring for most undergoing the surgery, it does not address the underlying cause.
In my practice, the uvula can return to normal size with anti-reflux treatment within weeks to months. The reason I show these photographs here in this blog is because to my knowledge these findings have never been reported in the medical literature.
For doctors, especially ENTs: The findings of silent long-standing silent nighttime reflux that cause both sleep apnea and snoring are: (1) cobble-stoning, erythyema and obliteration of the fossa of Rosenmuller (photo not shown), (2) a narrow granular pharynx, (3) an enlarged uvula, (4) thick mucus in the nose and throat, and (5) swelling of the back part of the larynx, the medical term of which is post-cricoid edema (shown below). Theoretically, swelling in this area helps keep reflux out of the lungs by creating a biologic barrier, like a levy.
The number one finding of nocturnal reflux is post-cricoid edema that is so swollen that it is in contact with the posterior pharyngeal wall (below).

For the average reader of this blog, these photographs may be meaningless or confusing. However, when your ENT doctor examines you – if you have snoring and/or sleep apnea — ask him whether these findings are present, because if they are, your snoring and sleep apnea are probably caused by reflux.
One final word about reflux and sleep. Even if you don’t have snoring sleep apnea, reflux can wake you up in the middle of the night coughing and gasping for air like a fish out of water. This is called a laryngospasm and it is a frightening symptom. Even if you don’t have laryngospasm, reflux can disrupt sleep. I cannot tell you how many of my patients tell me how much better they sleep once their reflux is controlled.
First, See If You Likely Have Reflux
The Koufman Reflux Symptom Index (RSI) is a proven tool to determine if you likely have acid reflux. Note that heartburn / indigestion is just one symptom in the index (which only 20% of refluxers experience).
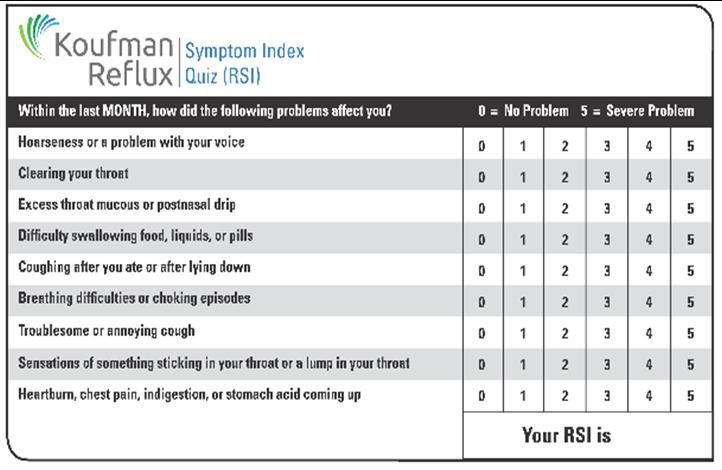
If you have an RSI score of 15 or greater, you have a 90% chance of having reflux, even if you have never had heartburn or indigestion. This is called silent reflux, and it’s very common.
Please understand that it’s important to take steps if you have reflux to manage it through lifestyle changes (explained later). If you let reflux run rampant, you’re setting yourself up for sleep apnea, COPD, chronic respiratory conditions, and a far higher risk of esophageal cancer.
Where to Get More Information
My best-selling book Dropping Acid with the companion book Dr. Koufman’s Acid Reflux Diet provide a comprehensive plan to start. If you’d like an initial primer on reflux, this article is also wonderful.
If you’ve read at least one of my books and you’re following my guidance and you still need help, you can book a consultation with me.
P.S. – Why Doesn’t My Doctor Know About This?
I get asked this all the time: “Why doesn’t my doctor know about this?!”
My primary research on acid reflux and chronic cough has been available for decades. Dropping Acid has been a best-seller for a decade. And I was on TV and quoted in mainstream media for many years. But the medical community remains virtually unaware that LPR (laryngopharyngeal reflux), today often called silent reflux or respiratory reflux (all terms I coined), is a major cause of respiratory issues and chronic cough. In addition, neurogenic cough seems almost never properly diagnosed.
Thousands of my patients have been on a merry-go-round of specialists… a GI doctor, an ENT, an allergist, an asthma specialist. They’ve had tens of thousands of dollars of tests, prescriptions for medications that never could have helped them, and their respiratory issues never improved.
The problem in the U.S. is over-specialization. Most Americans mistakenly believe that they must see specialists for almost every medical problem. What people don’t know is that specialists determine what services insurance will pay the most for, and they can choose to deliver those expensive services… even for patients who don’t need them! The idea of dividing the body up into small, non-overlapping, anatomic areas makes no sense. The respiratory and digestive systems are intimately connected, and specialists do not seem to know that.
Imagine building a house by allowing each workman to do his own thing. The plumber would put a sink in every room. The electrician would install chandeliers on every ceiling. The carpenter would panel every room in luxurious wood. That’s how America’s medical specialist system works.
The evolution of my personal medical practice as an expert in acid reflux that affects the throat and airway (LPR, silent reflux, respiratory reflux – all terms that I coined) helped me see that silent respiratory reflux was ubiquitous. That means it’s all over the place, and it’s likely in almost half of Americans. REFLUX is the single most common cause of “allergies,” “asthma,” “sinus disease,” true sleep apnea, and chronic cough.
Please read up and advocate for yourself, finding solutions that may be elusive through traditional care channels.