At-A-Glance
- According to the Asthma and Allergy Foundation of America, 25 million people (1:13) have asthma; of those, 80% are adults, and African-Americans are 55% more likely to have it than whites. Surprisingly, the annual price tag for “asthma” is $82 billion.
- The majority of people with “asthma” don’t have it. Four red flags for asthma misdiagnosis are: (1) During the “asthma” attack, the sufferer has trouble breathing IN (not out); (2) Without any airway obstruction, shortness of breath is not asthma; (3) chronic cough isn’t asthma either, and (4) if your asthma medications don’t work, it may be an alternative diagnosis, like respiratory reflux (LPR).
- Most acute breathing problems are caused by respiratory reflux, and it’s often “silent,” that is, occurring without telltale GERD symptoms like heartburn and indigestion. Most physicians are essentially unaware of this type of reflux, being handicapped by persistent misinformation from gastroenterologists who focus almost exclusively on esophageal reflux disease.
- WAKE UP CALL: Physicians tend to diagnose a wide array of breathing problems as “asthma” even if the symptoms don’t fit. The information in this blog (especially the IN-vs-OUT paradigm) should be known by every physician. Trouble breathing OUT is asthma; trouble breathing IN is reflux.
- Based upon four decades of experience, I believe that approximately 80% of patients with “asthma” don’t have it. Perhaps if this was known, we might save $55 billion a year on “asthma” and more importantly, people with breathing problems might then receive proper diagnoses and effective treatments.
- How does all this apply to you? See Think About Your Bottom Line at the bottom of this post.
The purpose of the post is to provide a wake-up call to people with “asthma” and their physicians.
In my practice over four decades, I have seen thousands of patients with “asthma” who simply didn’t have it. Such patients usually report that their asthma medications do nothing (with the possible exception of albuterol inhalers). And furthermore, they don’t have difficulty getting air OUT of the lungs with expiratory wheezing, the diagnostic sine qua non for asthma. If they have any airway obstruction, it is almost always inspiratory, IN, getting air into to the lungs.
I am amazed by physician ignorance. One patient reported that she told her pulmonologist that inspiratory breathing problems were reflux and not asthma, and he was amazed and thankful for the “new” information. Why did he not know this most basic fact about airway compromise? Trouble breathing IN is associated with an above-the-chest level of obstruction, and trouble breathing OUT is associated with obstruction within the chest … with reflux and asthma being the most common respective diagnoses. This is just basic physiology.
What Is Asthma?
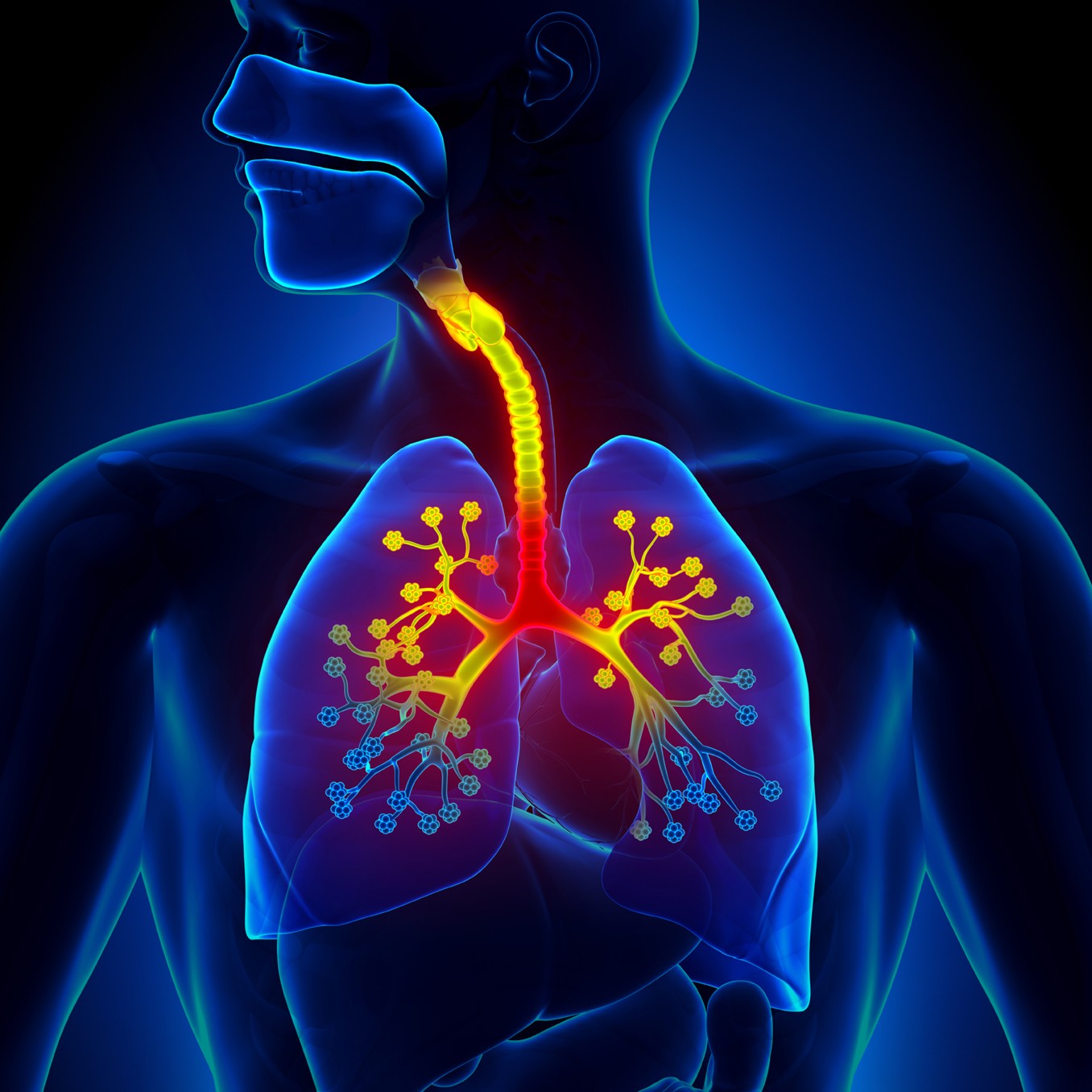
Asthma is a medical condition in which the airways within the lungs swell and narrow; the medical terms for this are bronchospasm and bronchoconstriction … literally meaning, the big breathing tubes in the lungs (bronchi) go into spasm and narrow. Only difficulty breathing OUT, during exhalation is asthma; anything else is not asthma.
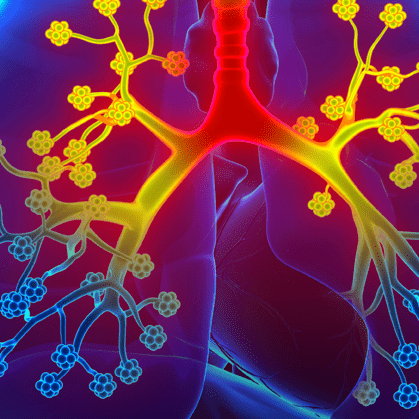
This photo shows what asthma looks like inside the lungs. The big tubes are the trachea and bronchi; and the red and yellow areas show where asthma constricts the most during an asthma attack. When one tries to exhale with this, chest muscle squeeze and compression of the chest further narrows the affected airways, increasing the difficulty getting air OUT of the lungs, often with wheezing … true asthma.
Narrowing of the airways within the lung makes exhalation difficult, prolonged and associated with noisy breathing (on exhalation), so-called wheezing. Shortness of breath and cough may be associated asthma; but remember, the number one symptom of asthma is trouble getting air OUT of the lungs.
The causes of true asthma include allergies, toxic fumes, and acid reflux, particularly respiratory reflux or LPR. This may surprise you, but reflux is the single most common trigger for true asthma attacks; see related bog on Exercise-Induced Reflux and Asthma. According to Dr. Sue Harding at UAB, as many as 70% of asthmatics have reflux as a trigger.
What About Acid Reflux and “Pseudo-Asthma”?
The answer in a word is: IN! Trouble breathing IN is almost always reflux, and never is it asthma.
Why trouble inhaling, breathing in? There is a vagally-mediated reflex that closes the vocal cords when acid (pH <2.5) stimulates (supraglottic) acid receptors on the top of the voice box. This closure of the vocal cords when partial is called paradoxical vocal cord movement, and when they clamp completely shut, that is called laryngospasm; those topics are additionally covered in the Choking Blog.

Reflux-Caused Paradoxical Vocal Cord Movement: The three photos from left-to-right are of a patient with reflux laryngitis and partial airway obstruction while inhaling. Under normal circumstances, the vocal cords open fully (like the left photo) when one is breathing IN; but in this case, the vocal cords are closing during IN-halation, as shown in the right-hand photo. You can judge the relative size of the airway by the dark center-portion that decreases in size from an open V (left) to a narrow oval (right). The right-hand photo shows this patient’s narrow airway during inspiration, which causes shortness of breath as well as inspiratory stridor, noisy breathing IN. This patient has respiratory reflux causing paradoxical vocal cord movement. Note: The term, “wheezing” is usually reserved for expiratory stridor seen in asthma.
Shortness of breath and cough without expiratory airway obstruction is not asthma. Again, respiratory reflux is the most common cause of shortness of breath and chronic cough with or without airway obstruction … not asthma! For more about chronic cough, see The Chronic Cough Enigma.
Notably, there is one peculiar breathing symptom that is virtually pathognomonic for respiratory reflux; it’s the inability to take a full breath of air IN … and this is not because of airway obstruction … inhaling deeply just doesn’t feel right.
What You and Your Doctor Should Know About Reflux & Asthma
Trouble breathing OUT is asthma; trouble breathing IN is reflux.
Respiratory reflux (RR), formally called Laryngopharyngeal Reflux (LPR) is acid reflux that comes up into the throat, and then may head north or south to affect any part of the respiratory system
RR is ubiquitous and it is the single most common trigger of true asthma attacks.
Overall, RR is the most common cause of shortness of breath, Airway Obstruction, Chronic Cough, Chronic Bronchitis, and COPD.
RR is often Silent Reflux, occurring without typical GERD symptoms of heartburn or indigestion.
RR is not in the curricula of most doctors today; and the “go-to” reflux doctor, the gastroenterologist, knows virtually nothing about RR … and has no tests or treatments for it. Generally-speaking, ENT doctors know more about RR than GI doctors, but ENT training in this area is still hit or miss.
Think About Your Bottom Line
If you have been diagnosed with “asthma,” ask yourself if during an asthma attack if you have more trouble breathing IN or OUT. Do you suffer from respiratory reflux (LPR) symptoms, like post-nasal drip, chronic throat clearing, globus, hoarseness, etc.? Are your asthma medications ineffective, NOT work?
If the answer is IN, and yesses for the other two questions, then you don’t have asthma, but rather respiratory reflux!!!