At-A-Glance
- Some symptoms just scream, RESPIRATORY REFLUX, but most people don’t know. How did I learn about these red flags? Experience with thousands of patients — always the best teachers.
- I believe that three-quarters of snoring and sleep apnea cases are reflux-caused, but it takes years, maybe decades of silent nocturnal respiratory reflux. Unfortunately, most people and their physicians are unaware of the underlying problem.
- To find out if you have reflux, I share “seven red flag symptoms.”
This article is excerpted from Dr. Koufman’s up-coming book, “Respiratory Reflux: How Silent Reflux Causes Disease,” due to be released in late 2023 or early 2024.
Note: Respiratory Reflux (RR) and Laryngopharyngeal Reflux (LPR) are synonyms and the terms can be used interchangeably. Going forward, I prefer the term RR and so should you; it is easier to pronounce, more intuitive, and implies that RR can affect any and all parts of the respiratory system which it does.
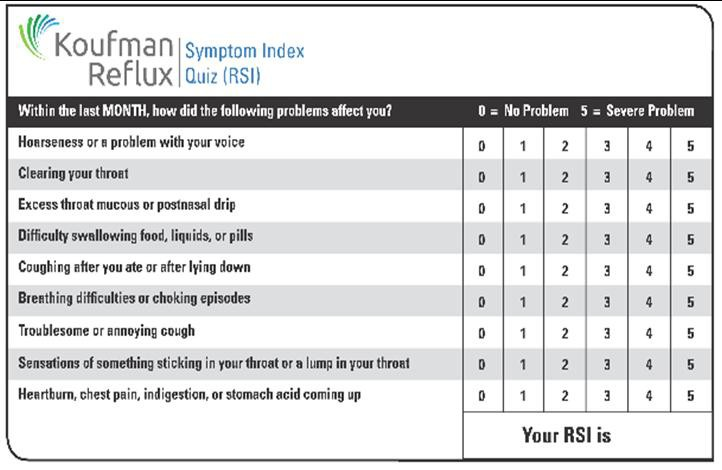
Silent Nocturnal Respiratory Reflux, also known as LPR (laryngopharyngeal reflux), is a type of reflux that occurs when stomach acid flows back up into the throat (pharynx) and voice box (larynx), without causing the typical symptoms of gastroesophageal reflux disease (GERD) such as heartburn. Take the conventional Reflux Symptom Index (RSI) that has been used as a reliable respiratory reflux measure for decades; and then, move on to the seven no-so-obvious “red flag” symptoms. If you have any of those (that often can be masquerading as other conditions), you need to consider silent reflux.
There are many symptoms and diseases where Respiratory Reflux, Silent Reflux may be the root cause … even some that might surprise you. However, from years of practice, I have learned that there are some symptoms that I call “red-flags,” symptoms that are strongly linked to respiratory reflux.
Seven Red Flag Symptoms
Trouble Breathing IN: You’ve been diagnosed as having asthma, but the medication doesn’t help much, and you have more trouble breathing IN, rather than out, that’s reflux, not asthma. Asthma is never a breathing-IN, inhalation problem. True asthma is characterized by trouble breathing OUT, getting the trapped air out of your lungs … difficulty getting the air OUT of your chest due to swollen bronchial tubes. Trouble breathing IN is reflux-related; see blog on asthma.
Comment: That most doctors don’t know this is shocking. Recently, after I stopped a patient’s “asthma” medication and fixed her reflux, she went to her pulmonologist and told him about the IN/OUT difference. He was grateful for the info, but I was amazed — every doctor should know this — it is based on airway anatomy and physiology and should be a medical school topic.
Unexplained Shortness of Breath: Unexplained shortness of breath (in a non-smoker), especially the inability to take in a full breath IN, or even do so uncomfortably. This is a very specific respiratory reflux symptom. It has never been reported in the literature, but it’s a common in my experience. It is vagally-mediated; but fix the reflux and it goes away.
Comment: When a person has shortness of breath, that symptom can take several forms: (1) Huffing and puffing after exertion, maybe even going up stairs, (2) True asthma or pseudo-asthma as above, (3) Airway obstruction, and (4) Inability or discomfort taking a full breath in. I always ask patients with shortness of breath to define the symptom. And when asked, most respiratory reflux patients who check off “shortness of breath” on their intake forms have the cant-take-a-full-breath-in symptom. Alas, I have never reported this in the medical literature, but how do you report an observation with no physical findings?.
Awakening in the night coughing and Coughing After Eating: In my experience, taken together, those two symptoms pretty much make the diagnosis of respiratory reflux, and severe reflux at that. This is non-pulmonary cough, not occurring because of a lung problem. This is not COPD or asthma; it’s REFLUX. If you awaken in the middle of the night coughing — BINGO! For more, you can read my blog on this topic or my book, The Chronic Cough Enigma. Or you can also book a virtual consultation with me to discuss your specific problem.
Comment: Cough is frequently misdiagnosed, but those who wake up in the middle of the night coughing sometimes breathing like a fish out of water ― that kind of choking episode is laryngospasm, when acid causes the vocal cords to clamp shut ― it is respiratory reflux. People with this problem should eat very early and sleep on a high incline, as well as tighten up on all the other antireflux measures recommended throughout this blog.
Globus | Sensation of A-lump-In-The-Throat: An annoying sensation of a lump in the throat that seems to be there all of the time, except when you’re eating. While eating, you may have difficulty swallowing. Read blog on globus for more. This means that the upper esophageal valve (UES) is out of whack from reflux; fix the reflux and the valve gets well and symptoms go away.
Comment: Interestingly, even in people who bitterly complain that the globus is constant, when asked, “Do you notice it when eating?” … most say NO … this is a diagnostic clinical pearl. Again, globus goes away when the reflux is treated. If there is a question of another diagnosis, especially if the patient also complains of significant difficulty swallowing, a barium swallow/esophagram x-ray is indicated as the first test.
Thick Mucus | Post-Nasal Drip: Thick mucus that is difficult to move and gets stuck on your vocal cords causing problems is almost exclusively reflux-related. I wrote a blog on too much mucus and post-nasal drip that might be helpful.
Comment: I am amazed at how frequently reflux is misdiagnosed as allergy. Allergies should be easily differentiated from reflux. Allergy mucus is thin, easy to move, and never gets on the vocal cords. On the other hand, respiratory reflux produces thick mucus, and that mucus is hard to move, especially when it gets on the vocal cords and reflux mucus is usually associated with chronic throat-clearing. Also people with allergies often have triggers, e.g., recently mowed grass, as well as other allergy symptoms such as nasal congestion, runny nose, and/or puffy, itchy eyes. Reflux and allergy are both common and some people have both.
Snoring | Sleep Apnea: This one will be controversial, but I’d bet the ranch on it. In reviewing clinical data, the majority of patients who snore and/or have sleep apnea also have silent respiratory reflux. There are findings in the throat that appear diagnostic. Also, too much surgery is being done on the palate and for big uvula. I have seen all return to normal with three weeks of tight antireflux treatment. I don’t know which is worse, the problem, or the fact that doctors are clueless that reflux is often causative. So yes, I have had patients reverse their snoring and sleep apnea with long-term therapy. Here we are talking a year.
Comment: I have been examining patients and doing reflux testing since the 1980s. In the last decade, there’s been a real up-tick in snoring and sleep apnea in my patients. Believe it or not every single one of them has similar findings in the throat, namely, a big uvula, a narrow, granular pharynx, as well as abnormal reflux-testing. It probably takes years of silent nocturnal respiratory reflux, perhaps decades, for snoring and sleep apnea to develop. The fact that this is unknown to most physicians, even sleep specialists, is a problem. I believe that at least three-quarters of people with snoring and sleep apnea have long-standing reflux as the cause.
Bitter Taste: A bitter taste in your mouth when you wake up in the morning or trouble with your gums and/or teeth as an adult is the ultimate form of reflux. Read my blog on dental problems and reflux for more.
Comment: If you awake in the morning with a bitter taste in your mouth, you know that you were refluxing all night. This can have serious effects on the gums and teeth and even cause a RAW kind of chronic sore throat. I consider bitter-taste-in-the-morning to be a serious reflux symptom.
What Should I Do if I Think I Have Reflux?
This blog has been written to provide the most up-to-date information that I can, and I urge you to explore it. On the left side on the blog page, there is a list of topics. In addition, there is a box that allows you to search any terms. I have written three books an acid reflux, particularly respiratory reflux (aka LPR): Dropping Acid, Dr. Koufman’s Acid Reflux Diet, and The Chronic Cough Enigma. I view the first two as companion books.
Is There a Cure for Acid Reflux?
Yes, but there is no medical solution, by that I mean that there is no pill or procedure that you can take that will vanquish reflux. Fix reflux? There is only one cure: diet and lifestyle modifications are absolutely necessary, and must be very strict at the beginning; see my YouTube Dr. K’s Reflux Detox or get my book Dr. Koufman’s Reflux Diet.